On a melancholy Saturday this past February, Shalon Irving's "village" — the friends and family she had assembled to support her as a single mother — gathered at a funeral home in a prosperous black neighborhood in southwest Atlanta to say goodbye.
The afternoon light was gray but bright, flooding through tall, arched windows and pouring past white columns, illuminating the flag that covered her casket. Sprays of callas and roses dotted the room like giant corsages, flanking photos from happier times: Shalon in a slinky maternity dress, sprawled across her couch with her puppy; Shalon, sleepy-eyed and cradling the tiny head of her newborn daughter, Soleil. In one portrait, Shalon wore a vibrant smile and the crisp uniform of the Commissioned Corps of the U.S. Public Health Service, where she had been a lieutenant commander. Many of the mourners were similarly attired. Shalon's father, Samuel, surveyed the rows of somber faces from the lectern. "I've never been in a room with so many doctors," he marveled. "... I've never seen so many Ph.D.s."
At 36, Shalon had been part of their elite ranks — an epidemiologist at the Centers for Disease Control and Prevention, the pre-eminent public health institution in the U.S. There she had focused on trying to understand how structural inequality, trauma and violence made people sick. "She wanted to expose how people's limited health options were leading to poor health outcomes," said Rashid Njai, her mentor at the agency. "To kind of uncover and undo the victim-blaming that sometimes happens where it's like, 'Poor people don't care about their health.' " Her Twitter bio declared: "I see inequity wherever it exists, call it by name, and work to eliminate it."
Much of Shalon's research had focused on how childhood experiences affect health later on — examining how kids' lives went off track, searching for ways to make them more resilient. Her discovery in mid-2016 that she was pregnant with her first child had been unexpected and thrilling.
Then the unthinkable happened. Three weeks after giving birth, Shalon collapsed and died from complications of high blood pressure.
The researcher working to eradicate disparities in health access and outcomes had become a symbol of one of the most troublesome health disparities facing black women in the U.S. today: disproportionately high rates of maternal mortality. The main federal agency seeking to understand why so many American women — especially black women — die, or nearly die from complications of pregnancy and childbirth had lost one of its own.
Even Shalon's many advantages — her B.A. in sociology, her two master's degrees and dual-subject Ph.D., her gold-plated insurance and rock-solid support system — had not been enough to ensure her survival. If a village this powerful hadn't been able to protect her, was any black woman safe?
The sadness in the chapel was crushing. Shalon's long-divorced parents had already buried both their sons; she had been their last remaining child. Wanda Irving had been especially close to her daughter — role model, traveling companion, emotional touchstone. She sat in the front row in a black suit and veiled hat, her face a portrait of unfathomable grief. Sometimes she held Soleil, fussing with her pink blanket. Sometimes Samuel held Soleil, or one of Shalon's friends.
A few of Shalon's villagers rose to pay tribute; others sat quietly, poring through their funeral programs. Daniel Sellers, Shalon's cousin from Ohio and the baby's godfather, spoke for all of them when he promised Wanda that she would not have to raise her only grandchild alone.

"People say to me, 'She won't know her mother.' That's not true," Sellers said. "Her mother is in each and every one of you, each and every one of us. ... This child is a gift to us. When you remember this child, you remember the love that God has pushed down through her for all of us. Soleil is our gift."
The memorial service drew to a close, the bugle strains of taps as plaintive as a howl. Two members of the U.S. Honor Guard removed the flag from Shalon's coffin and held it aloft. Then they folded it into a precise triangle small enough for Wanda and Samuel to hold next to their hearts.
Racial disparity across incomes
In recent years, as high rates of maternal mortality in the U.S. have alarmed researchers, one statistic has been especially concerning. According to the CDC, black mothers in the U.S. die at three to four times the rate of white mothers, one of the widest of all racial disparities in women's health. Put another way, a black woman is 22 percent more likely to die from heart disease than a white woman, 71 percent more likely to perish from cervical cancer, but 243 percent more likely to die from pregnancy- or childbirth-related causes. In a national study of five medical complications that are common causes of maternal death and injury, black women were two to three times more likely to die than white women who had the same condition.
That imbalance has persisted for decades, and in some places, it continues to grow. In New York City, for example, black mothers are 12 times more likely to die than white mothers, according to the most recent data; in 2001-2005, their risk of death was seven times higher. Researchers say that widening gap reflects a dramatic improvement for white women but not for blacks.
The disproportionate toll on African-Americans is the main reason the U.S. maternal mortality rate is so much higher than that of other affluent countries. Black expectant and new mothers in the U.S. die at about the same rate as women in countries such as Mexico and Uzbekistan, the World Health Organization estimates.
What's more, even relatively well-off black women like Shalon Irving die and nearly die at higher rates than whites. Again, New York City offers a startling example: A 2016 analysis of five years of data found that black, college-educated mothers who gave birth in local hospitals were more likely to suffer severe complications of pregnancy or childbirth than white women who never graduated from high school.
The fact that someone with Shalon's social and economic advantages is at higher risk highlights how profound the inequities really are, said Raegan McDonald-Mosley, the chief medical director for Planned Parenthood Federation of America, who met her in graduate school at Johns Hopkins University and was one of her closest friends. "It tells you that you can't educate your way out of this problem. You can't health care-access your way out of this problem. There's something inherently wrong with the system that's not valuing the lives of black women equally to white women."

For much of American history, these types of disparities were largely blamed on blacks' supposed susceptibility to illness — their "mass of imperfections," as one doctor wrote in 1903 — and their own behavior. But now many social scientists and medical researchers agree, the problem isn't race but racism.
The systemic problems start with the type of social inequities that Shalon studied — differing access to healthy food and safe drinking water, safe neighborhoods and good schools, decent jobs and reliable transportation.
Black women are more likely to be uninsured outside of pregnancy, when Medicaid kicks in, and thus more likely to start prenatal care later and to lose coverage in the postpartum period. They are more likely to have chronic conditions such as obesity, diabetes and hypertension that make having a baby more dangerous. The hospitals where they give birth are often the products of historical segregation, lower in quality than those where white mothers deliver, with significantly higher rates of life-threatening complications.
Those problems are amplified by unconscious biases that are embedded in the medical system, affecting quality of care in stark and subtle ways. In the more than 200 stories of African-American mothers that ProPublica and NPR have collected over the past year, the feeling of being devalued and disrespected by medical providers was a constant theme.
There was the new mother in Nebraska with a history of hypertension who couldn't get her doctors to believe she was having a heart attack until she had another one. The young Florida mother-to-be whose breathing problems were blamed on obesity when in fact her lungs were filling with fluid and her heart was failing. The Arizona mother whose anesthesiologist assumed she smoked marijuana because of the way she did her hair. The Chicago-area businesswoman with a high-risk pregnancy who was so upset at her doctor's attitude that she changed OB/GYNs in her seventh month, only to suffer a fatal postpartum stroke.
Over and over, black women told of medical providers who equated being African-American with being poor, uneducated, noncompliant and unworthy. "Sometimes you just know in your bones when someone feels contempt for you based on your race," said one Brooklyn, N.Y., woman who took to bringing her white husband or in-laws to every prenatal visit. Hakima Payne, a mother of nine in Kansas City, Mo., who used to be a labor and delivery nurse and still attends births as a midwife-doula, has seen this cultural divide as both patient and caregiver. "The nursing culture is white, middle-class and female, so is largely built around that identity. Anything that doesn't fit that identity is suspect," she said. Payne, who lectures on unconscious bias for professional organizations, recalled "the conversations that took place behind the nurse's station that just made assumptions; a lot of victim-blaming — 'If those people would only do blah, blah, blah, things would be different.' "
In a survey conducted this year by NPR, the Robert Wood Johnson Foundation and the Harvard T.H. Chan School of Public Health, 33 percent of black women said that they personally had been discriminated against because of their race when going to a doctor or health clinic, and 21 percent said they have avoided going to a doctor or seeking health care out of concern they would be racially discriminated against.
Black expectant and new mothers frequently said that doctors and nurses didn't take their pain seriously — a phenomenon borne out by numerous studies that show pain is often undertreated in black patients for conditions from appendicitis to cancer. When Patrisse Cullors, a co-founder of the Black Lives Matter movement who has become an activist to improve black maternal care, had an emergency C-section in Los Angeles in March 2016, the surgeon "never explained what he was doing to me," she said. The pain medication didn't work: "My mother basically had to scream at the doctors to give me the proper pain meds."
But it's the discrimination that black women experience in the rest of their lives — the double whammy of race and gender — that may ultimately be the most significant factor in poor maternal outcomes.

"It's chronic stress that just happens all the time — there is never a period where there's rest from it. It's everywhere; it's in the air; it's just affecting everything," said Fleda Mask Jackson, an Atlanta researcher who focuses on birth outcomes for middle-class black women.
It's a type of stress for which education and class provide no protection. "When you interview these doctors and lawyers and business executives, when you interview African-American college graduates, it's not like their lives have been a walk in the park," said Michael Lu, a longtime disparities researcher and former head of the Maternal and Child Health Bureau of the Health Resources and Services Administration, the main federal agency funding programs for mothers and infants. "It's the experience of having to work harder than anybody else just to get equal pay and equal respect. It's being followed around when you're shopping at a nice store, or being stopped by the police when you're driving in a nice neighborhood."
An expanding field of research shows that the stress of being a black woman in American society can take a physical toll during pregnancy and childbirth.
Chronic stress "puts the body into overdrive," Lu said. "It's the same idea as if you keep gunning the engine, that sooner or later you're going to wear out the engine."
As women get older, birth outcomes get worse. ... If that happens in the 40s for white women, it actually starts to happen for African-American women in their 30s.
Arline Geronimus, a professor at the University of Michigan School of Public Health, coined the term "weathering" for stress-induced wear and tear on the body. Weathering "causes a lot of different health vulnerabilities and increases susceptibility to infection," she said, "but also early onset of chronic diseases, in particular, hypertension and diabetes" — conditions that disproportionately affect blacks at much younger ages than whites. Her research even suggests it accelerates aging at the molecular level; in a 2010 study Geronimus and colleagues conducted, the telomeres (chromosomal markers of aging) of black women in their 40s and 50s appeared 7 1/2 years older on average than those of whites.
Weathering has profound implications for pregnancy, the most physiologically complex and emotionally vulnerable time in a woman's life. Stress has been linked to one of the most common and consequential pregnancy complications, preterm birth. Black women are 49 percent more likely than whites to deliver prematurely (and, closely related, black infants are twice as likely as white babies to die before their first birthday). Here again, income and education aren't protective.
The repercussions for the mother's health are also far-reaching. Maternal age is an important risk factor for many severe complications, including pre-eclampsia, or pregnancy-induced hypertension. "As women get older, birth outcomes get worse," Lu said. "If that happens in the 40s for white women, it actually starts to happen for African-American women in their 30s."
This means that for black women, the risks for pregnancy start at an earlier age than many clinicians — and women— realize, and the effects on their bodies may be much greater than for white women. In Geronimus' view, "a black woman of any social class, as early as her mid-20s should be attended to differently."
That's a concept that professional organizations and providers have barely begun to wrap their heads around. "There may be individual doctors or hospitals that are doing it [accounting for the higher risk of black women], but ... there's not much of that going on," Lu said. Should doctors and clinicians be taking into account this added layer of vulnerability? "Yeah," Lu said. "I truly think they should."

A high-pressure life
Shalon Irving's history is almost a textbook example of the kinds of strains and stresses that make high-achieving black women vulnerable to poor health. The child of two Dartmouth graduates, she grew up in Portland, Ore., where her father's father was pastor of a black church. Even in its current liberal incarnation, Portland is one of the whitest large cities in the U.S., in part a vestige of the state's founding by Confederate sympathizers who wrote exclusion of blacks into their constitution.
Thirty years ago, Portland was a much more uncomfortable place to be black. African-American life there was often characterized by social isolation, which Geronimus' research has shown to be especially stressful. Her father, Samuel Irving, spent years working for the railroad and later for the city but felt his prospects were limited by his race. Her mother, Wanda Irving, held various jobs in marketing and communications, including at the U.S. Forest Service. In elementary school, Shalon was sometimes the only African-American child in her class. "There were many mornings where she would stand outside banging on the door wanting to come back into the house because she didn't want to go to school," her mother recently recalled.
Shalon's strategy for fitting in was to be smarter than everyone else. She read voraciously, wrote a column for a black-owned weekly newspaper, and skipped a grade. Books and writing helped her cope with trauma and sorrow — first the death of her 20-month-old brother Simone in a car accident when she was 6, then the fracturing of her parents' marriage, then the diagnosis of her beloved older brother, Sam III, with a virulent form of early-onset multiple sclerosis when he was 17. Amid all the family troubles, Shalon was funny and driven, with a fierce sense of loyalty and "a moral compass that was amazing," her mother said.
She was also overweight and often anxious, given to daydreaming (as she later put it) about "alternative realities where people hadn't died and things had not been lost." When it came time to go away to college, she chose the historically black Hampton University in Virginia. "She wanted to feel that nurturing environment," Wanda said. "She had had enough."
By then, Shalon had noticed that many of her relatives —her mother's mother, her aunts, her far-flung cousins — had died in their 30s and 40s. Her brother Sam III sardonically joked that the family had a "death gene," but Shalon didn't think that was funny. "She didn't understand why there was such a disparity with other families that had all these long lives," Wanda said. Shalon nagged her father to stop smoking and her mother to lose weight. She set an example, shedding nearly 100 pounds while managing to graduate summa cum laude. At the start of graduate school at Purdue University, she was a svelte 138 pounds, "very classy and elegant, a lot like her mom," said Bianca Pryor, a master's student in consumer behavior who became one of her closest friends.

West Lafayette, Ind., felt as white as Portland. For support, Shalon relied on a cherished circle of "sister friends," as she called them. "There's this feeling that we're carrying the expectations of generations, the first ones trying to climb the corporate ladder, trying to climb in academe," Pryor said. "There is this idea that we have to work twice as hard as everyone else. But there's also, 'I'm first-generation; I don't know the ropes; I don't how to use my social capital.' There's a bit of shame in that ... this constant checking in with yourself — am I doing this right?"
Much of Shalon's pressure was self-imposed: She was pursuing a double Ph.D. in sociology and gerontology, focusing on themes she would return to often — the long-term effects of early-childhood trauma and maltreatment, the impact of the parent-child relationship on lifelong health. She finished in under five years, once again with highest honors — "one of the best writers I've had in my academic career," her adviser, sociologist Kenneth Ferraro, said.
Next, Shalon decided to pursue a second master's degree, this time from Johns Hopkins. She was also juggling family responsibilities. Wanda had followed Shalon around the country, working in nonprofit management. "They were like the Gilmore Girls," Pryor said. In 2008, Sam III joined them in Baltimore to take part in a study for an experimental MS therapy. With his family's support, he had managed to finish college and run a poetry-slam nonprofit for kids. His next goal was to walk across the stage to receive his diploma instead of using his wheelchair. In February 2009, while he was doing physical rehab to regain strength in his legs, a blood clot traveled to his lung, killing him at the age of 32. Afterward, Wanda and Shalon clung to each other more tightly than ever.

What Shalon wasn't prepared for was how unfulfilled she was. After Johns Hopkins, she had worked on the front lines helping at-risk infants, teenage girls, and mothers with HIV/AIDS. She was passionate about improving food and housing security to reduce people's risk for high blood pressure and other cardiovascular problems. At the CDC, it bothered her that she rarely met the people behind the data she was analyzing. As a consultant for Michelle Obama's anti-obesity initiative Let's Move! "she might see the numbers, but I don't think she actually saw that little girl or little boy have a healthier lunch," Pryor said.
The stress and frustration triggered the old corrosive self-doubts. But gradually, Shalon saw a way out of the box. She joined the CDC's Division of Violence Prevention, refocusing on issues around trauma and domestic abuse — a mission she saw as "liberating" for African-American women, Wanda said. She started a coaching business called Inclusivity Standard to advise young people from disadvantaged backgrounds who wanted to get into college or grad school and organizations seeking to become more diverse. And she decided to write a self-help book, on the theory that many people in the communities she cared about couldn't afford psychotherapy or didn't trust it. "She was one of those people — one thing is just not enough," said her co-author, Habiba Tran, a therapist and life coach with a multicultural clientele. "One modality is just not enough. One way of [reaching people] is just not enough."

Becoming a mother
Shalon couldn't remember a time when she didn't want to be a mother. But her romantic life had been a "20-year dating debacle," she admitted in the manuscript of her self-help book, in part because "I am deathly scared of heartbreak and disappointment, and letting people in comes with the very real risk of both."
In 2014, when Shalon was 34, medical problems forced the issue. For years she had been suffering from uterine fibroids — nonmalignant tumors that affect up to 80 percent of black women, leading to heavy menstrual bleeding, anemia and pelvic pain. No one knows what causes fibroids or why blacks are so susceptible. What is known is that the tumors can interfere with fertility — indeed, black women are nearly twice as likely to have infertility problems as whites, and when they undergo treatment, there's much less likelihood that the treatments will succeed. Surgery bought her a little time, but her OB/GYN urged her not to delay getting pregnant much longer.
Shalon had spent her adult years defying stereotypes about black women; now she wrestled with the reality that by embracing single motherhood, she could become one. The financial risk was substantial — she had just purchased a town house in the quiet Sandy Springs area north of Atlanta, and her CDC insurance covered artificial insemination only for wives using their husbands' sperm. In Portland, no one would have blinked an eye at an unmarried professional woman having a child on her own, but in Atlanta, "there is very much a vibe there that things should happen in a certain order," Pryor said. "And Shalon was not having that at all. She was like, 'Nope, this is what it is.' "
The gamble — funded with her parents' help — ended in a series of devastating failures. In September 2015, in the midst of an unsuccessful fertility treatment, Shalon was alarmed to discover that her right arm had become swollen and hard. Doctors found a blood clot and diagnosed her with Factor V Leiden, a genetic mutation that makes blood prone to abnormal clumping. Suddenly a part of the family's medical mystery was solved. Wanda's mother had died of a pulmonary embolism; so had Sam III; so had other members of their extended family. But no one had been tested for the mutation, which is primarily associated with European ancestry. Had they known they carried it, maybe Sam's deadly blood clot could have been prevented. It was a what-if too painful to dwell on.
By April 2016, Shalon had given up. She had a new boyfriend and was on her way to Puerto Rico to help with the CDC'S Zika response, working to prevent the spread of the virus to expectant mothers and their unborn babies. There, she discovered she'd gotten pregnant by accident. Her excitement was tempered by fear that the baby might have contracted Zika, which can cause microcephaly and other birth defects. But a barrage of medical tests confirmed all was well.
More good news: A few weeks later, her friend Pryor learned she was pregnant, too. "All right," she told Shalon, "let's finally go after our rainbows and unicorns! Because for so long it was just dark clouds and rain."

In reality, Shalon's many risk factors — including her clotting disorder, her fibroid surgery, the 36 years of wear and tear on her telomeres, her weight — boded a challenging nine months. She also had a history of high blood pressure, though it was now under control without medication. "If I was the doctor taking care of her, I'd be like, 'Oh, this is going to be a tough one,' " her OB/GYN friend McDonald-Mosley said.
Shalon got through the physical challenges surprisingly well. Her team at Emory University, one of the premier health systems in the South, had no trouble managing her clotting disorder with the blood thinner Lovenox. They worried that scarring from the fibroid surgery could result in a rupture if her uterus stretched too much, so they scheduled a C-section at 37 weeks. At several points, Shalon's blood pressure did spike, Wanda said, but doctors ruled out pre-eclampsia and the numbers always fell back to normal.
Wanda blamed stress. There was the painful end to Shalon's romance with her baby's father and her dashed hopes of raising their child together. There were worries about money and panic attacks about the difficulties of being a black single mother in the South in the era of Trayvon Martin and Tamir Rice. Shalon told everyone she was hoping for a girl.
Steeped in research about how social support could buffer against stress and adversity, Shalon joined online groups for single mothers and assembled a stalwart community she could quickly deploy for help. "She was all about the village," Njai, her CDC mentor, said. "She'd say, 'I'm making sure that when I have my baby, the village is activated and ready to go.' "
She poured more of her anxious energy into finishing the first draft of the book. She sent Tran the manuscript on Jan. 2, the day before the planned C-section, then typed one last note to her child. Boy or girl, its nickname would be Sunny, in honor of her brother Sam, her "sunshine." "You will always be my most important accomplishment," she wrote. "No words have been created to adequately capture the fear and love and excitement that I feel right now."
Sporadic postpartum care
Until recently, much of the discussion about maternal mortality has focused on pregnancy and childbirth. But according to the most recent CDC data, more than half of maternal deaths occur in the postpartum period, and one-third happen seven or more days after delivery. For American women in general, postpartum care can be dangerously inadequate — often no more than a single appointment four to six weeks after going home.
"If you've had a cesarean delivery, if you've had pre-eclampsia, if you've had gestational diabetes or diabetes, if you go home on an anticoagulant — all those women need to be seen significantly sooner than six weeks," said Haywood Brown, a professor at Duke University medical school. Brown has made reforming postpartum care one of his main initiatives as president of the American Congress of Obstetricians and Gynecologists.
The dangers of sporadic postpartum care may be particularly great for black mothers. African-Americans have higher rates of C-section and are more than twice as likely to be readmitted to the hospital in the month following the surgery. They have disproportionate rates of hypertensive disorders and peripartum cardiomyopathy (pregnancy-induced heart failure), two leading killers in the days and weeks after delivery. They're twice as likely as white women to have postpartum depression, which contributes to poor outcomes, but they are much less likely to receive mental health treatment.
If they experience discrimination or disrespect during pregnancy or childbirth, they are more likely to skip postpartum visits to check on their own health (they do keep pediatrician appointments for their babies). In one study published earlier this year, two-thirds of low-income black women never made it to their doctor visit.
Meanwhile, many providers wrongly assume that the risks end when the baby is born — and that women who came through pregnancy and delivery without problems will stay healthy. In the case of black women, providers may not understand their true biological risks or evaluate those risks in a big-picture way. "The maternal experience isn't over right at delivery. All of the due diligence that gets applied during the prenatal period needs to continue into the postpartum period," said Eleni Tsigas, executive director of the Preeclampsia Foundation.
All of the due diligence that gets applied during the prenatal period needs to continue into the postpartum period.
It's not just doctors and nurses who need to think differently. Like a lot of expectant mothers, Shalon had an elaborate plan for how she wanted to give birth, even including what she wanted her surgical team to talk about (nothing political) and who would announce the baby's gender (her mother, not a doctor or nurse). But like most pregnant women, she didn't have a postpartum care plan. "It was just trusting in the system that things were gonna go OK," Wanda said. "And that if something came up, she'd be able to handle it."
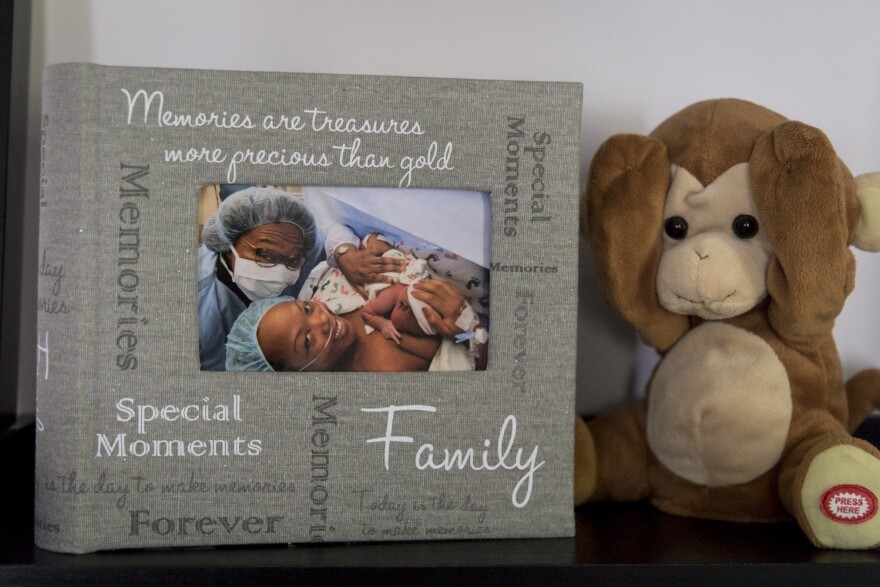
The birth was "a beautiful time," Wanda said. Shalon did so well that she persuaded her doctor to let her and Soleil — French for "sun" — leave the hospital after two nights (three or four nights are more typical). Then at home, "things got real," Pryor said. "It was Shalon and her mom trying to figure things out, and the late nights, and trying to get baby on schedule. Shalon was very honest. She told me, 'Friend, this is hard.' "
C-sections have much higher complication rates than vaginal births. In Shalon's case, the trouble — a painful lump on her incision — started a week after she went home. The first doctor she saw, on Jan. 12, said it was nothing, but as she and her mother were leaving his office, they ran into her regular OB/GYN, Elizabeth Collins, whom Shalon trusted completely. Collins took a look and diagnosed a hematoma — blood trapped in layers of healing skin, something that happens in about 1 percent of C-sections. She drained the "fluctuant mass" (as her notes described it), and "copious bloody non-purulent material" poured out from the 1-inch incision. Collins also arranged for a visiting nurse to come by the house every other day to change the dressing.
What troubled the nurse most, though, was Shalon's blood pressure. On Jan. 16 it was 158/100, high enough to raise concerns about postpartum pre-eclampsia, which can lead to seizures and stroke. But Shalon didn't have other symptoms, such as headache or blurred vision. She made an appointment to see the OB/GYN for the next day, then ended up being too overwhelmed to go, the visiting nurse noted on Jan. 18. In that same record, the nurse wrote that Shalon had to change the dressing on her wound "sometimes several times a day due to large amounts of red drainage. This is adding to her stress as a new mom." Her pain was 5 on a scale of 10, preventing her from "sleeping/relaxing." Overall, Shalon told the nurse, "it just doesn't feel right." When the nurse measured her blood pressure on the cuff Shalon kept at home, the reading was 158/112. On the nurse's equipment, the reading was 174/118.
Under current ACOG guidelines, those readings were high enough to warrant more aggressive action, Tsigas said, such as an immediate trip to the doctor for further evaluation, possibly medication, and more careful monitoring. That is especially true for someone with a history of hypertension and multiple other risks. "We need to look holistically at the risk factors irrespective of whether or not she had a diagnosis of pre-eclampsia," Tsigas said. "If somebody has a whole plateful of risk factors, how are you treating them differently?"
"It would have made sense to admit her to the hospital for a complete work-up," including chest X-ray, an echocardiogram to evaluate for heart failure, and titration of her medication to get her blood pressure to normal range, wrote one doctor, a leading expert on postpartum care, who agreed to look at Shalon's records at ProPublica's request but asked not to be identified. The doctor said that the communication about signs of stroke seemed insufficient and that it would be more "common practice" to assess her that day to find out what was wrong.
Instead, Shalon was given an appointment for the next day, Jan. 19, with an OB/GYN at Women's Center at Emory St. Joseph's, which handled her primary care. By then, Shalon's blood pressure had fallen to 130/85 — considered on the high end of normal — and there were "no symptoms concerning for postpartum [pre-eclampsia]," the doctor wrote in his notes. He wrote that Shalon was healing "appropriately" and thought her jumps in blood pressure were likely related to "poor pain control." Wanda and Shalon left feeling more frustrated than ever.
At home over the next couple of days, Wanda noticed that one of Shalon's legs was larger than the other. "She said, 'Yeah, I know, Mom, and my knee hurts, I can't bend it.' "
When McDonald-Mosley looked over the voluminous medical records a few months later, what jumped out at her was the sense that Shalon's caregivers (who declined to comment for this story) didn't seem to think of her as a patient who needed a heightened level of attention, despite the complexity of her pregnancy.
"She had all these risk factors. If you're gonna pick someone who's going to have a problem, it's gonna be her. ... She needs to be treated with caution." The fact that her symptoms defied easy categorization was all the more reason to be vigilant, McDonald-Mosley said. "There were all these opportunities to identify that something was going wrong. To act on them sooner and they were missed. At multiple levels. At multiple parts of the health care system. They were missed."
Shalon's other friends were growing uneasy, too. Pryor had her own pregnancy emergency — her son was born very prematurely, at 24 weeks — so she couldn't be in Atlanta. But she and Shalon talked often by phone. "She knew so much about her body one would think she was an M.D. and not a Ph.D. To hear her be concerned about her legs — that worried me." Pryor encouraged her, " 'Friend, are you getting out of the house? Are you going for your walks?' She told me, 'No, I'm on my chaise lounge, and that's about as much as I can do.' "
Life coach Tran was so upset at Shalon's condition that she took her frustrations out on her friend. "I was cussing her out. 'Go to the f****** doctor.' She's like, 'I called them. I talked to them. I went to see them. Get off my back.' "

"There is something wrong"
On the morning of Tuesday, Jan. 24, Shalon took a selfie with her father, who had been visiting for a few days, then sent him to the airport to catch a flight back to Portland. Toward noon, she and Wanda and the baby drove to the Emory Women's Center one more time. This time, Shalon saw a nurse practitioner. "We said, 'Look, there's something wrong here; she's not feeling well,' " Wanda recalled. " 'One leg is larger than the other; she's still gaining weight — 9 pounds in 10 days — the blood pressure is still up. There's gotta be something wrong.' "
The nurse's notes confirmed Shalon had swelling in both legs, with more swelling in the right one. She noted that Shalon had complained of "some mild headaches" but didn't have other worrisome symptoms, like blurred vision. She checked the incision — "warm dry no [sign/symptom] of infection" — and noted Shalon's mental state ("cooperative, appropriate mood & affect, normal judgment").
" 'You guys have to realize she just had a baby. Don't worry about it, things are calming down,' " Wanda recalled the nurse telling them. " 'We'll send her down for an ultrasound to see if she has a clot in her leg.' " Shalon's blood pressure was back up to 163/99, so the nurse also ordered a pre-eclampsia screening.
Both tests came back negative. "So they're saying, 'Well if there's no clots, there's nothing wrong,' " Wanda recalled. As Wanda remembers it, Shalon was insistent: "There is something wrong, I know my body. I don't feel well, my legs are swollen, I'm gaining weight. I'm not voiding. I'm drinking a lot of water, but I'm retaining the water." As Wanda recalls it, the nurse told them, "There is nothing we can do; you just have to wait, give it more time." Before sending Shalon home, the nurse gave her a prescription for the blood pressure medication nifedipine, which is often used to treat pregnancy-related hypertension.

Shalon and Wanda stopped at the pharmacy, then decided to go out to dinner with the baby. While they ate, they talked about a trip Shalon had planned for the three of them to take in just a few weeks. Ever since Sam III had died, Wanda and Shalon had made a point of traveling someplace special on painful anniversaries. To mark his 40th birthday and the eighth anniversary of his death, Shalon had gotten the idea of going to Dubai. ("It's cheap," Shalon had told Wanda. "The money is worth so much more there. It's supposed to be beautiful.") She had long ago purchased their tickets and ordered the baby's passport. Now Wanda was worried — would she be feeling well enough to make such a big trip with an infant? Shalon wasn't willing to give up hope just yet. Wanda recalls her saying, "I'll be fine, I'll be fine."
They got home and sat in Shalon's bedroom for a while, laughing and playing with the baby. Around 8:30 p.m., Shalon suddenly declared, "I just don't know, Mom, I just don't feel well." She took the blood pressure medication from Wanda and got ready for bed. An hour later, Wanda heard a terrifying gasping noise. Shalon had collapsed.
The news spread quickly among her colleagues at the CDC. William Callaghan, chief of the maternal and infant health branch, recalled in March that his boss, who had visited Shalon at the hospital, called to let him know. "It was a chilling phone call," said Callaghan, one of the nation's leading researchers on maternal mortality. "It certainly takes, in that moment, what I do, it made it very, very, very concrete. ... This was not about data, this was not about whether it was going up or it was going down. It was about this tragic event that happened to this woman, her family."
Northside decided against an autopsy, telling Wanda and Samuel that there was nothing unusual about Shalon's death, they recalled. (The hospital declined to comment.) So Wanda paid $4,500 for an autopsy by the medical examiners in neighboring DeKalb County. The report came back three months later. Noting that Shalon's heart showed signs of damage consistent with hypertension, it attributed her death to complications of high blood pressure.

Raising Soleil
Wanda moved into Shalon's tidy town house to care for Soleil. Even though Shalon's villagers fulfilled their pledges at the memorial service, coming by often to give Wanda a break, the first months were borderline unbearable — the baby was colicky, prone to gastric problems that kept both of them up all night. Wanda's grief was endless, bottomless, but she couldn't let it interfere with her duties to Soleil. "She's the only reason I get up every morning, pretty much," Wanda said.
Eventually the colic went away and Soleil thrived. In June, Wanda and her 5-month-old granddaughter drove to Chattanooga, Tenn., for the annual meeting of U.S. Public Health Service scientists. A new honor — the Shalon Irving Memorial (Junior) Scientist Officer of the Year Award — had been created to celebrate Shalon's legacy, and Wanda had been asked to say a few words. She handed the baby to one of Shalon's CDC colleagues and took the small stage.
"Striving for excellence is a choice," she told the audience through barely suppressed tears. "It is a commitment. ... It's a struggle to become the person you want to be. It's harder than you want. It takes longer than you want. And it takes more out of you than you expected it should."
Shalon personified excellence, Wanda said. "I don't know if Shalon became the woman that she ultimately wanted to be. But I do know that she wanted to be the woman she was."

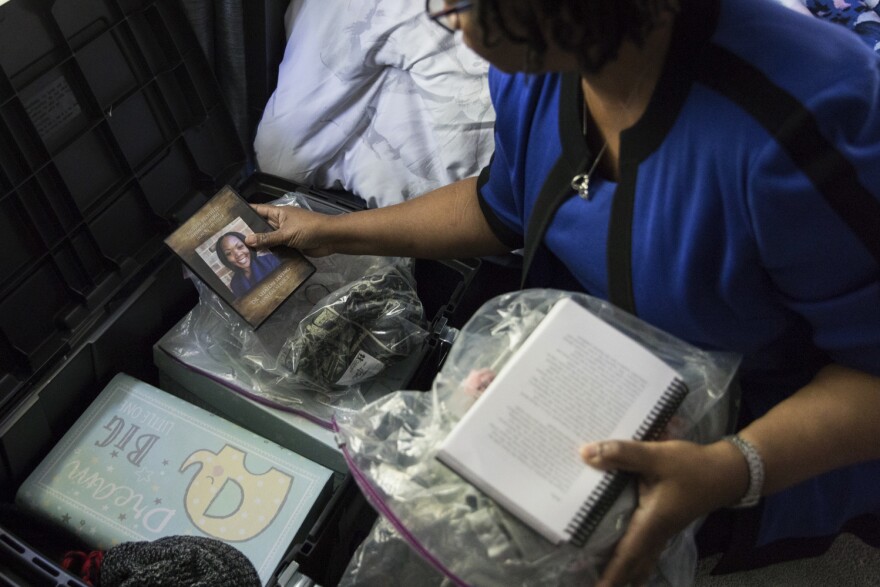
One Saturday afternoon in October, Wanda received a book that friends of Shalon's from the Epidemic Intelligence Service had compiled, titled Letters to Soleil. She put Soleil on her lap and said, "I'm gonna read you some letters about your mom." One thing Wanda has tried never to do is cry in front of Soleil. But as she began reading the letters, she was sobbing. "And Soleil just kept looking at me — she couldn't understand what was going on. And about a minute later she took my glasses off with her hands and put them down and then laid her head right on my chest and started patting me. Which made me cry all the more."
As Soleil got older, Wanda looked forward to doing the kinds of things with her that Shalon had looked forward to: reading to her, traveling with her, taking her to gymnastics and music classes. "She wanted Soleil to go to Montessori school, so I'm looking for a Montessori school for her," Wanda said. "She wanted her to be christened; we got her christened."
Now 10 months old, Soleil has her mother's eyes, energy and headstrong yet sweet disposition, coming into Wanda's bed every night and waking her early to play. "She'll bite my nose and kick me — 'Nana, time to get up! Time to get up!' That's what keeps me motivated."
A week or so after the memorial service, Wanda came across a letter that Shalon had written to her two years earlier, around the sixth anniversary of Sam III's death. Shalon had left it among the other important items on her computer, trusting that if something ever happened to her, Wanda would find it. The letter reads like a premonition: Shalon was contemplating the prospect of her own premature death — and of her beloved mother having to endure one more unbearable tragedy.
I am sorry that I have left you. On the particular day that I am writing this I have no idea how that may have occurred but know that I would never choose to leave.
I know it seems impossible right now, but please do not let this break you. I want you to be happy and smile. I want you to know that I am being watched after by my brothers and grandma and that we are all watching you. Please try not to cry. Use your energy instead to feel my love through time and space. Nothing can break the bond we have and you will forever be my mommy and I your baby girl!
Copyright 2023 NPR. To see more, visit https://www.npr.org.




